OverDiagnosed: Making People Sick in Pursuit of Health
As if the earth itself had shook, tremors of fear rippled through the rocky-edged terrain of our nervous system. My wife, Sonia, had gone for her annual mammography with expectations of the usual “we’ll see you next year” routine. Not this time. They wanted to take a second look not only with a mammogram (X rays that photograph the breasts to detect malignancies), but also a sonogram, whose sound waves can detect abnormalities.
The tendency is to fear the worst notwithstanding that there are so many “false positive” readings that occur with these tests. So after taking more time off from work and following the usual pre-exam instructions, we hurried back to the radiological center for a second look. As Sonia was escorted into the examination room, I was left in the waiting area to browse through those annoying magazines that obsessively chronicle America’s celebrity culture, steal a furtive glance at other patients dutifully filling out the required medical forms, and compulsively look at the clock every 5 minutes leading me to conclude that time does not fly, it downright crawls.
The wait was interminable. Finally, like a prisoner awaiting the verdict of the jury, they came for me. I met Sonia in a long and winding hallway and we were promptly ushered into a spacious, sunlit office with walls that reflected a collage of dulcet, comforting colors. Sitting with his back toward us behind a broad and imposing mahogany desk was the radiologist. His gaze focused intently, almost hypnotically on the photographs on his computer screen. I felt apprehensive, uncertain but tried to look reassuringly at Sonia. Without turning around, he gently told us to sit in the plump, attractively upholstered chairs that faced his desk. Frankly, I didn’t want to sit down but I thought it rude to reject the invitation and besides, such a recalcitrant posture in the face of common courtesy might unnecessarily alarm my dear wife. Smiling weakly, I turned toward her about to gesture that we sit when I saw she had already exercised that liberty and was lounging comfortably in its cushioned seat. For a second, I felt strangely unneeded.
After another excruciating minute, the doctor told us that things looked good and summoned us to view the images that had so feverishly consumed his attention. His manner turned from studious to pleasant and even gracious. He pointed out the density of the fibroids that had aroused suspicions, but almost jauntily concluded they were probably not malignant. “Probably” was the operative word and one that filled me with an inquisitive uneasiness. “Well, doctor,” I stammered, “exactly what do you mean when you say probably? Shouldn’t these tests definitively put the question to rest?” Pausing momentarily, he responded with the tentativeness of a man cracking eggshells: “Essentially that’s true, they should,” the doctor opined, “but it’s not absolutely true.” “Uh huh, not absolutely true,” I mindlessly repeated, “well then would you say (grasping at a courtroom analogy) that the possibility of malignancy is “beyond all reasonable doubt?” The open-face, sunny smile of the radiologist began to fade like light before the approaching dusk. “I’m saying Mr. Guarnieri,” (the way he accentuated the vowels in my name only a dolt could not have perceived an acid crispness had injected itself in the dialogue) “that the only way one could be 100 percent sure of such a diagnosis is to do a biopsy.” “Are you saying then,” I persisted, “that it is your professional opinion that a biopsy is required?” “Well, as I said if you want to be 100 percent sure the answer is yes.”
I was about to say something about the preponderance of evidence when I felt that all too familiar kick in the shin from my wife and realized my semantic duel with the doctor had come to a screeching, if not, unceremonious halt. I had reservations but readily ceded to my wife’s wishes to have a biopsy. More instructions: no aspirin a week before the procedure — fear of bleeding — more time off from work — more worrying. The procedure was briefer than I thought although it entailed for Sonia some discomfort, a little pain, inconvenient bandaging (when is it ever convenient?), black and blue discoloring and, of course, more than a touch of anxiety. Everything, fortunately, came back benign.
Nonetheless, I began to ponder the despotism of modern medicine. There was a time people only went to doctors when they perceived something wrong — being sick was one good indication. The emphasis is now on prevention; the evolution of medical technology has made it so. The advances in radiological imaging, magnetic resonance imaging as well as the ultrasound and imaging I haven’t even heard of has provided the medical community a window of the inner workings of our bodies with a resolution and clarity that a previous generation of clinicians could barely imagine. No wonder that in the United States the number of MRI and CT exams per capita is more than double the average of industrial countries. Everyone wants the comfort of being sure. But while these exams provide real benefits in particular cases, the aggregate health benefits have no documentable advantage. Screening for colon cancer is recommended once every five years for everyone 50 years old and more frequently for those with risk factors. However, 90 percent of these procedures routinely turn up nothing.
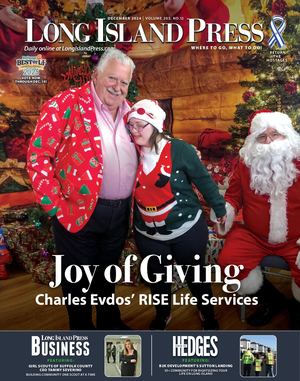
It’s not my position that these procedures should be discontinued; only that what has been an evolutionary leap for medical science, a haven for hypochondriacs, has not been an altogether salubrious development for the person who is relatively healthy. Perhaps it hasn’t been a completely positive experience for anyone. I have a friend who seeks medical attention when he has a runny nose; a certified hypochondriac — it’s in his Last Will and Testament that he be buried next to his doctor. These sophisticated tests, however, have nursed rather than diminished his neurotic fixations. These images, after all, can detect the slightest abnormality from the tiniest blood clots in the lungs and legs to innocuous cysts domiciled in the breasts, borderline aneurysms and a host of other imperfections. A recent book on the subject, authored by physicians Welch, Schwartz and Woloshin titled, OverDiagnosed: Making People Sick in Pursuit of Health argues that the quest to find potential disease has entrenched itself into the medical culture often leading to unnecessary medication and surgery.
My doctor, an offbeat medic, has some unconventional views regarding the practice of medicine. When you mention prostate tests to detect cancer, he thunders: “An utterly useless test, but I order it anyway because it looks good in court.” To me this is a common sense approach; why run to a doctor when you’re asymptomatic. This might appear at variance with my reactions to my wife’s mammography experience but this is because I’m not especially solicitous about my own health, only those I love. Whatever my idiosyncrasies, the testing of healthy patients inevitably leads to over-diagnosis and overtreatment especially in light of the shifting numbers of what is normal and abnormal in terms of blood pressure and cholesterol counts. Thirty years ago the norm was notably higher than it is today.
As medical technology advances and with genetic medicine on the horizon, a spirited debate will serve as an important counterweight, a healthy (no pun intended) dose of skepticism regarding the overall effectiveness as well as the downside of medical testing that becomes ubiquitous when the better choice for prevention is a sound diet, regular exercise, the avoidance of tobacco and proper rest. These things are available to all and it’s the best medicine we can take.