Preparedness is the best remedy for Ebola
Winthrop University Hospital hosted a presentation on the current Ebola epidemic, at the Garden City Library, on Tuesday, Nov. 11. Sponsored by the village’s Property Owners’ Associations, John F. Collins, president and CEO of Winthrop University Hospital and Dr. Michael Ammazzalorso, Winthrop’s Chief Medical Officer provided an overview of the disease along with an update on Winthrop’s preparedness plan.
Dr. Ammazzalorso began his presentation heeding that despite the waning in the press, the disease is still with us. He provided both historical and current day perspectives regarding the epidemic, advising that Ebola is not a new disease. The medical community has been aware of the disease for at least 40 years. Originating in the Congo, Ebola is a zoonosis a disease which has its reservoir in animals and was known for small sporadic outbreaks associated with people who handled bats and rodents or those who consumed bush meat. The current outbreak originated in West Africa, specifically Sierra Leone, Guinea and Liberia. He noted in Africa that more than 45,000 people have died from the disease.
“Thankfully there are no current active cases in the United States that we know of,” said Dr. Ammazzalorso. “Preparedness is half the battle.”
Dr. Ammazzalorso provided further insight into symptoms and facts concerning Ebola. Those who have no symptoms can’t spread the disease. If exposed to the disease, symptoms appear within 8-12 days after exposure and include: fever, chills, malaise, fatigue, muscle aches and headaches. Late stage symptoms present as severe watery diarrhea, vomiting, loss of appetite, rash, pink eye, spontaneous bleeding and multi-organ failure. The current course of treatment is to provide fluids, oxygen, nutrition and treatment of secondary bacterial infections. Care is limited due to protective gear and precautions prevent even stethoscope use.
“Mr. Duncan, who died in Dallas, died as a result of kidney shut down,” advised Dr. Ammazzalorso. “There is reason for concern, 72 percent of those contracting the disease die from it…patients over age 45 have a higher incidence of fatalities.”
However Dr. Ammazzalorso added: “Many more people will die from complications from influenza in this country than will die from Ebola, so this is a very good reason for getting the influenza vaccine. You will be doing yourself a great favor if you get the flu vaccine.”
He highlighted Duncan’s case. Though two nurses, who treated him, contracted the disease, so many others such as family, close contacts and patients in the hospital waiting room, where he was treated several times, did not contract the disease.
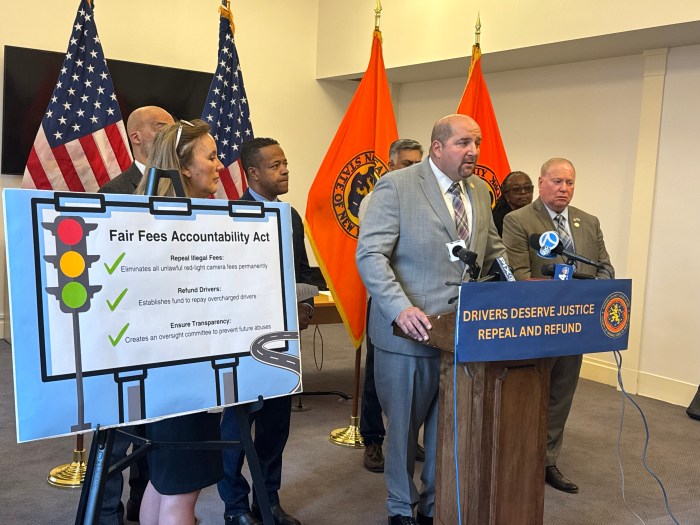
Collins provided a snapshot of the days leading to the media hysteria and Winthrop procedures established to date.
“Much of the care for people who are under investigation is directed by the Department of Health (DOH),” said Collins. “If someone is identified as someone at risk, we isolate and then inform DOH and Centers for Disease Control (CDC). Every hospital needs to be prepared. On October 16, the acting commissioner of health in New York State, gave all hospitals and covered entities including diagnostic treatment centers, ambulance companies and funeral homes ten days to get ready. Mandates included establishing two contacts available 24/7, providing protective clothing, training and maintaining logs of all activity. Winthrop is currently in full compliance.”
Though regional centers have been established for Ebola patients, hospitals throughout the country may care for patients before diagnosis since blood testing can take 24 to 48 hours. Winthrop has established a containment approach. When a patient arrives at Winthrop’s emergency room, they are greeted by a registered nurse who establishes the patient’s symptoms and finds out if the patient has traveled to West Africa. If a possible case is established, an internal communication device alerts hospital personnel and a path is cleared for the patient to be escorted to a separate corridor to a designated isolation room. The room has been built so employees can change protective gear. Airborne precautions have been established to protect health care workers. The patient will stay in isolation and all laboratory testing and treatment will be accomplished in that section. If Ebola is confirmed, the patient would be sent to Glen Cove Hospital, which has been designated as a treatment center.
“I did not buy into a fire brigade approach, that is to train every single person in the hospital and six months from now we finally have a patient,” said Collins. “We have adopted a special teams approach for the environmental people, security, emergency room personnel and physicians who are routinely trained. I think most of the hospitals in the United States, and certainly New York State, are much more prepared now than they were before.”