As Covid-positive patients stream steadily into hospitals, a pandemic weary Long Island can count on its own health care heroes who put their own safety aside to carry them through. Some stand out as winners of the 2021 Bethpage Best of Long Island contest.
The winners include Medford Volunteer Ambulance, which won the title of Best Medical Transportation Company on Long Island, and Stony Brook University Hospital, which won the title of Best Maternity Ward on Long Island.
Each of these health organizations rose to the top in their response to Covid from the onset and their medical and supportive personnel displayed their outstanding skills, fortitude, and temperament to save and impact lives. So, what defines a health care hero? Read on to see what these outstanding institutions and their top-notch staff have in common.
Health care heroes agree that fighting Covid-19 requires a teamwork approach not only for the health of their patients but to support one another emotionally.
BEST MATERNITY WARD
Stony Brook University Hospital Preserves Joy And Wonderment of Childbirth
Expectant mothers arrive at Stony Brook University Hospital maternity ward surrounded by a caring and highly skilled staff of health care professionals who feel uniquely privileged to experience the miracle of childbirth with families.
The hospital has all private rooms and mothers and babies remain together as much as possible. Patients arriving at the hospital are tested for Covid-19. Covid-19 positive patients are cared for in negative pressure rooms in labor and delivery and staff closely monitor for signs and symptoms.
However, there were a few severe cases where the patients required a higher level of care in other areas of the hospital.
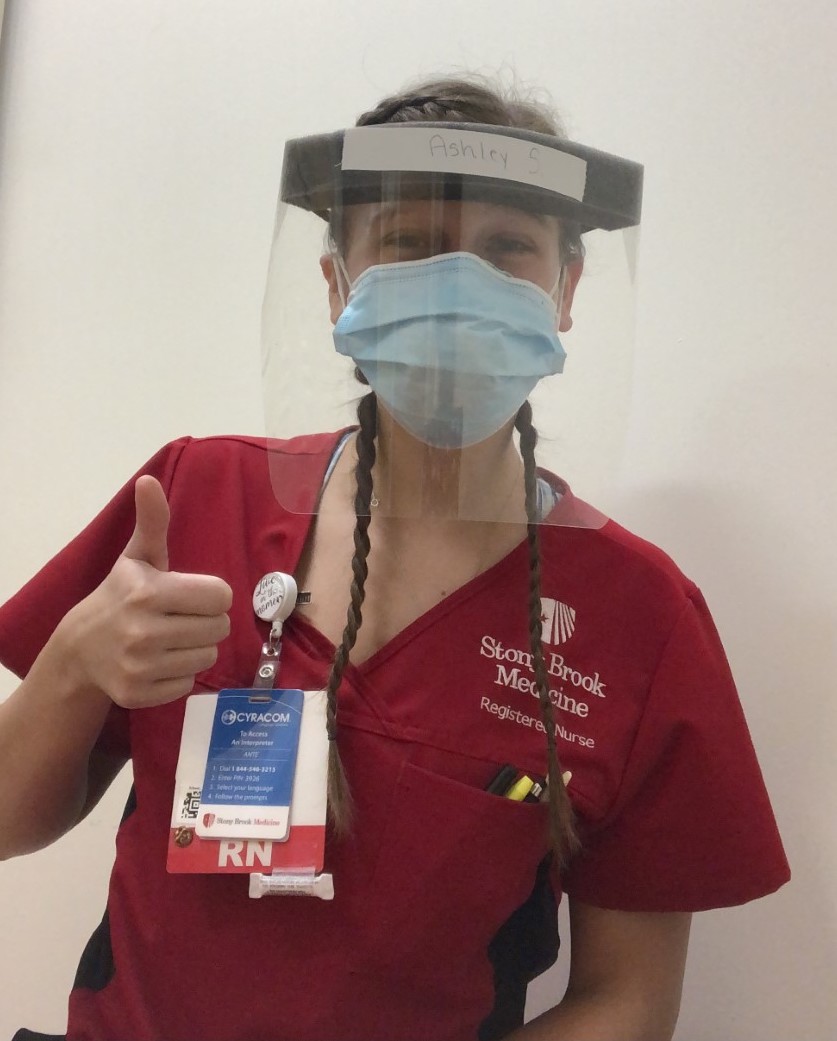
RN Ashley Schuette works in antepartum, labor and delivery, newborn and postpartum at Stony Brook Hospital. She recently talked about the benefits of expectant moms being able to have the company of a support person to stay with them throughout their birth experience, along with a doula if they want, for labor and delivery.
“Stony Brook did a great job because the moms were allowed to designate someone to come with them to the hospital and stay the entire time. We were great to be able to do that for our patients,” said Schuette in a phone interview.
Over the past year, some patients had Covid-19 but were asymptomatic and others were scared to get sick or have their babies get sick, she related.
“It’s different than before because you never know who is sick so you want to be careful around everyone. In the beginning, we didn’t know how it was affecting moms and babies and we could only go by what we were hearing from the CDC. It was scary for the patients. A new mom just wants to protect her baby and is nervous something will happen to their baby but they know we are doing our best.”

To assuage concerns among the expectant mothers she tries to educate them with information available from the CDC and hospital protocol to keep them safe.
According to Schuette, apart from the safety measures and donning the PPE for deliveries new moms enjoy the same joyous experience at Stonybrook.
She feels privileged to do the kind of work she does. “It’s one of the most rewarding things. You get to be a part of such an instant moment in people’s lives. You are there the first time they get to hear their baby cry. It’s incredible. Some [women] don’t think they can get through [labor] and they do.”
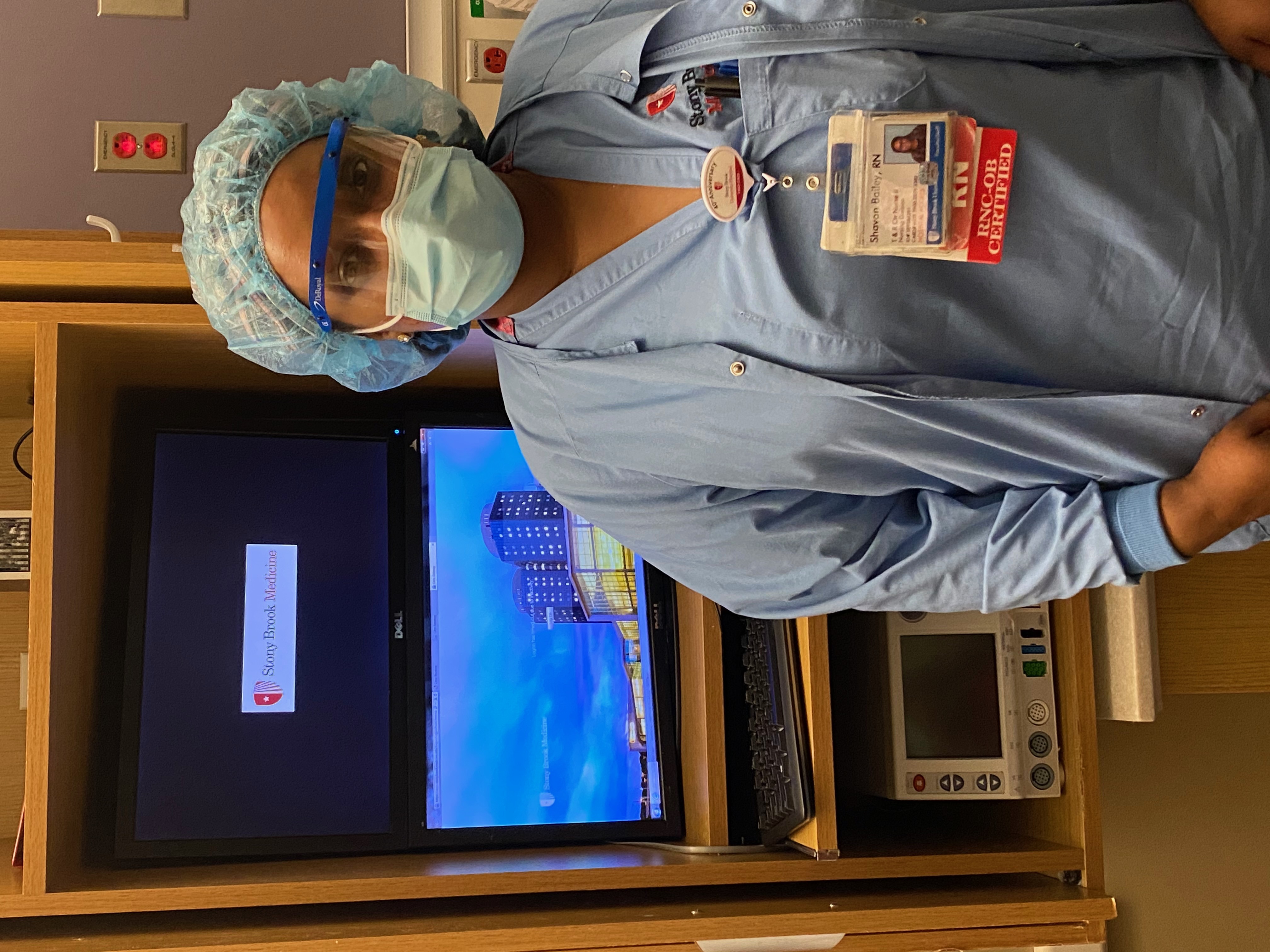
Shavon Bailey is also a nurse in antepartum, labor and delivery, newborn nurse, and postpartum. She talked about helping the mothers feel safe both before and during their stay at the hospital.
“Some are “nervous” about getting sick. We do our best from answering calls ahead of time and comfort them when they walk in the door. We listen to their concerns and answer questions, letting them know we are doing our best. We’re all good at comforting this way because this is our specialty.”
Bailey was one of the nurses at the hospital’s first Covid -19 C-section of a mom who was in the ICU, she related. “The mom was well and the baby was well and didn’t have Covid. We had great leaders that came up with the procedures and we practiced. It looked different with all the PPE and safety but it went very well.”
Labor and delivery nurse Elena Lecrichia recently gained a better understanding of what it is like to deliver a baby in a pandemic. She gave birth at Stony Brook in May. “My coworkers are capable of empathy and it gave me a personal edge to the experience,” she recounted.
She was seven months pregnant when news of Covid-19 hit.
In the beginning, she said there was general fear among herself and co-workers when like the rest of the world news of Covid-19 and how contagious it was began coming.
“It started off slow. There definitely was some fear. We’d hear about it a little bit then there were more and more patients coming in with Covid and you knew this is serious. This is contagious and no one wanted to bring that home to their family,” she recounted.
Lecrichia back then being pregnant added some concern for her at work. “We didn’t know if it would transmit to the baby. The fear was the unknown. It was hard,” Lecrichia said.
But she pushed through, and in fact, worked up until the day before her baby was born. Her coworkers were supportive. “We always wore the PPE and I always felt safe. And they took the assignments that were riskier, the patients with Covid.”

She agrees the best way to ease any concerns for pregnant women arriving to have their babies is through education and communication. “We work hard to normalize the process. Even though it’s during a pandemic and there’s more PPE for you it’s still going to be a loving experience,” said Lecrichia.
The new moms she’s seen coming through the doors are resilient. “They are amazing and can adapt to anything. I’m really impressed with our community of moms. Even though the world may look a little chaotic, it’s still a time to celebrate happy moments.”
BEST MEDICAL TRANSPORTATION COMPANY
Medford Volunteer Ambulance Brings Pre-Hospital Care, Comfort To Patients In Pandemic
Medford Volunteer Ambulance EMTs rely on teamwork and each other to answer the public’s call in the crisis – bringing emergency care and comfort in pre-hospital transport – making sure each patient has the best chance for recovery.
Volunteer EMT Justin Zimmerman credits a “close-knit” group among the volunteers who get each other through many of the unique and often difficult challenges in Covid-19 like when patients are critical and don’t survive and feeling worried about their own safety.
“In the beginning, I was trying to manage my time here and being around my family members. We all have older family members and people who are immune-compromised. It was about keeping them safe. A lot of us have lost family members to Covid,” he said in an interview.

The EMTs in the company are friends and work together on calls so share this observation, according to Zimmerman.
“Covid is a scary thing but we have to put our fears aside. This is what we signed up to do and have to help the community we said we would.”
Zimmerman also feels the mass media attention on healthcare workers during this pandemic can sometimes confuse people about the work of EMTs.
“The public is seeing what we do. Yes, we’re dealing with Covid but the emergencies are the same as EMTs do on a daily basis, the same that have been handled as long as there have been medical professionals,” he said. Emergency calls to administer lifesaving treatments to people dying from cardiac arrest is a common type of case, especially in Medford where there are several nursing homes nearby.
“A lot of times it happens because of the condition of their medical health. If we pull up the medical history they might have had Covid, and it was six months ago so the information is skewed toward that issue. It’s really hard to determine why that individual might have died,” he explained. Deaths and causes of death are handled by medical examiners not EMTs.
“We do get a lot of nursing home calls now like we always have. It’s relatively the same in terms of the patients but the difference is the facilities are calling us more and more, wanting us to take them to the hospital for treatment they can’t provide.”
The emphasis on the emergency calls is helping the patient and family be calm, Zimmerman said.
“We try to reassure them. A lot of times we get to the houses and they don’t want to go to the hospital. They are afraid. We know it’s a scary situation and there are bad outcomes so they need reassurance. The families are stressed because their family member has been sick and has a lot of issues. Now with Covid being in the mix, the families are freaking out. They don’t know how safe the hospitals are. They worry will the family member get Covid? A lot of the public is in the dark. To have the unknown is what really scares them.”
The EMTs follow New York State guidelines for transporting Covid-19 patients, explained First Assistant Chief John Skippon.
“We have a protocol to ask certain questions to see if a patient meets the criteria to go to the hospital that includes things like if they need oxygen and other emergency care. When a patient is Covid-19 positive the volunteers going on the call have to wear jumpsuits along with the N95 mask and goggles and one EMT goes into the home to minimize the risk to others unless it is an emergency, then all go in,” he said. The team effort begins before the call when “They help each other get into their jumpsuits.”
EMT Brianna Manganaro said 2020 was “rough.” Nursing school. “At the hospital, they get intubated and die and I also see others get extubated and go home,” she related.
As an EMT it helps to have friends on calls, she continued.
“At first we were uneasy. We were trying to comfort the patients. We have cried, also happy tears. You see [patients] at their worst. Justin [Zimmerman], Mike, and I are best friends,” Manganaro related.

Mike Hannan is a volunteer EMT in Medford and a New York City firefighter and used to transport dying patients. He said the Medford crew go out to the nursing homes four or five times a day some days.
“There was a little bit of fear at the beginning of Covid from going into people’s houses. Halfway through I got used to it,” he said.
“I’ve been exposed to a lot of more scary and dangerous situations than having to deal with Covid. In the beginning, we didn’t know enough about it and would worry about being exposed,’ he said. Hannan wound up getting the virus and was sick with all the symptoms, he said. Sadly, his father too contracted Covid and had to be put on a ventilator and died in January.
“Everybody is scared when they first contract [Covid-19]. In Suffolk County, we have a protocol in place for the pandemic to take them to the hospital. If we transport someone it’s because their vital signs are not good. You can see the fear in their eyes. I feel for the patients. I can understand where they’re coming from. There were a couple of times I was thinking this is not good.”
The more experience EMTs have they get used to it. I’ve been an EMT for 12 years. I feel bad for the family members of the patients for what they have to deal with. But I’ve become callous because of so many cardiac arrest calls, he said.
Teamwork is the most important part of the emergency calls, Manganaro explained.
“We know what to do next because we all know each other. You already know it can be a sad outcome. You have to push through anyway. You see negative outcomes more than positive,” Manganaro had Covid with few symptoms. Her grandmother died from Covid-19.
“You treat every patient like it’s your own family member,” she said.
For more coronavirus coverage, visit longislandpress.com/coronavirus.
Sign up for Long Island Press’ email newsletters here. Sign up for home delivery of Long Island Press here. Sign up for discounts by becoming a Long Island Press community partner here.