If you have trouble sleeping at night, you are not alone. Nearly three in 10 American adults (28%) said insomnia has a negative impact on their daily lives, according to an American Academy of Sleep Medicine study conducted earlier this year.
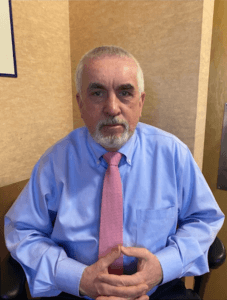
“Many people don’t think to go to a sleep specialist for a sleep problem – they just accept it or resign themselves to it,” said Lauren Broch, Ph.D., a behavioral sleep psychologist at the Northwell Health Sleep Disorders Center in New Hyde Park. “But there are a lot of things that can be done to help.”
Expert Advice for Better Sleep

Chronic Insomnia
Everyone has the occasional bad night’s sleep. But some people struggle on a regular basis to fall or stay asleep, or they wake up too early and can’t fall back asleep. When insomnia occurs at least three times a week for three months or longer, it’s considered chronic.
Chronic insomnia often begins with an acute episode caused by a stressful event, such as a job change, a death in the family, an illness, or a trip that removes you from your own familiar environment.
“As a result of the acute episode, you may develop behaviors related to poor sleep, such as getting on your phone at night or having negative thoughts, such as ‘I’m never going to get to sleep, and I’m going to be exhausted tomorrow,’” said Heidy Merius, D.N.P., a cognitive behavioral therapy for insomnia (CBTI) provider at the Stony Brook University Sleep Disorders Center in Smithtown.
Over time, negative thoughts and habits can lead to chronic insomnia.
“The more you worry about it, the worse it gets,” said Brendan Duffy, director of sleep services for Catholic Health, who is based at the health system’s St. Charles Sleep Disorders Center in Port Jefferson. “You get on a train going in the wrong direction.”
Other Sleep Disorders
Some people who struggle to get solid sack time have another underlying sleep disorder. There are about 80 sleep disorders in all, and obstructive sleep apnea and restless legs syndrome are among the most common. Obstructive sleep apnea is caused when the muscles in your throat relax during sleep and block or narrow your airway. Symptoms may include gasping for air while sleeping, snoring, daytime sleepiness, and problems with concentration. Uncontrolled sleep apnea increases your risk of high blood pressure and has been associated with other health problems. Restless legs syndrome (RLS) causes irresistible urges to move your legs, which can make it difficult to fall or stay asleep. RLS is more common in women and with increasing age, and it may be associated with low iron levels.
Sleep Center Evaluation
Depending on how your insurance works, you can go directly to a sleep center or be referred by your general practitioner.
“We typically start with an hour-long evaluation,” Broch said. “We ask patients about their sleep issues, their sleep habits, what time they’re getting into and out of bed, about their daytime functioning, mood, family history, medical history, and medications.”
Patients will be asked about other complaints, such as if they wake up gasping for air, if their partner says they snore, or if they are bothered by restless legs. When sleep apnea or another sleep disorder is suspected, patients may be evaluated with an overnight sleep study at the sleep center.
Sleep apnea can also be evaluated with a home-based sleep study, but a test done at the center is more comprehensive and accurate. Some insurance companies, however, will require you to take the home sleep study first to see if it detects apnea before they cover a center-based test, Merius said. Patients who are diagnosed with sleep apnea are often prescribed a continuous positive airway pressure (CPAP) machine.
Cognitive Behavior Therapy for Insomnia
Many sleep centers offer cognitive behavior therapy for insomnia, which involves relaxation techniques, cognitive restructuring, changing habits around bedtime, and restricting time in bed. Patients typically come for six to eight therapy sessions, which may or may not be covered by insurance.
“We advise patients to make their bedroom only for sleep – it’s not for paying bills, talking on the phone to friends, or watching TV,” Broch said.
Merius said she will look at the total amount of time a patient slept compared to the total amount of time spent in bed over a two-week period.
“They may be spending nine hours in bed a night, but only sleeping six hours,” she said. “In this case, we’ll have them restrict their time in bed to six hours.”
Since people with insomnia often spend a lot of time in bed worrying and trying to fall asleep, the goal with sleep restriction, according to Duffy, is to “get you to associate your time in bed with sleeping and not with angst.”
Duffy also encourages patients to be consistent about their wake-up times.
“People like to sleep in on weekends,” Duffy said. “It’s OK to sleep a little longer, but not too late.”
Avoiding caffeine late in the day, exercising, and getting outside early in the day are also recommended, Duffy said. It also helps to have a bedtime routine, similar to a morning routine.
“Just like you set an alarm in the morning, set an alarm one to two hours before bedtime, when you can start the down-ramp process,” he said. “When you fly a plane, you don’t just land it and it’s over – there’s a process.”