Everything we take and use for medicine has gone through a clinical trial, but fewer than 10 percent of Americans participate in them. And for those who might have heard the phrase “clinical trial,” 55 percent of Americans feel there is a lack of information—even if they want to participate.
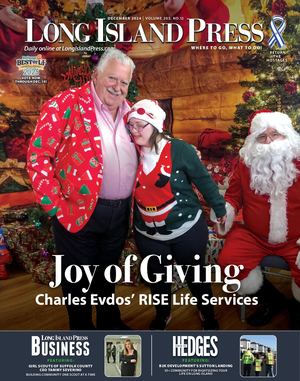
To help the community understand why clinical trials are so important, The Feinstein Institutes for Medical Research at Northwell Health hosted its first in-person Clinical Trials Day event at Adelphi University. Information tables and free resources were available, along with discussion panels from five New Yorkers who decided to better their health and participate in a clinical trial to help advance medical breakthroughs.
The event was hosted by Dr. Christina Brennan, the Senior Vice President for clinical research at Northwell. She oversees the clinical research program throughout Northwell’s 21 hospitals and ambulatory centers. “We wanted the opportunity to recognize clinical trial participants who have been in trials with us at Northwell, community members who wanted to learn more about clinical trials, as well as our workforce of clinical research professionals who work on the clinical trials at Northwell,” Brennan said.
Clinical trials, at their most basic, are tests to see if a drug, device or therapy is beneficial. Most people are somewhat familiar with the idea of testing drugs for their safety and effectiveness. “Clinical trials look at new ways, or expanded ways, to prevent, detect, control or treat disease, with the goal being to find if a new test or therapy is safe and effective,” said Brennan.
It is critically important that clinical trials include as many different kinds of people as possible in order to really provide an accurate picture of how effective the treatment is, as well as its side effects. “We’ve talked about for years, and even more so around the pandemic, how important it is to have many types of people with different ages, races, ethnicities and genders to see how these different treatments affect those different groups,” said Brennan.
Clinical Trials Day—a day dedicated to learning and recognizing professionals and their contributions to public health and medicine—is held on May 20 every year and commemorates the day that James Lind began the first randomized clinical trial in 1747—one that would help find new ways to treat sailors’ scurvy.
James Lind, a Scottish physician, was a pioneer of hygiene in the Royal Navy. After conducting one of the first-ever clinical trials, he developed the theory that citrus fruits cured scurvy.
Lind thought that scurvy could be helped by acids, so he included an acidic dietary supplement in the experiment. He divided twelve sick sailors into groups of two. They all received the same diet, but each group received a different treatment. Only the group getting citrus fruits improved. In 1753, he published a treatise on scurvy, which was mostly ignored. Fortunately for many sailors, the results of his experiment were eventually acknowledged, and the practice of clinical trials was born.
Even today, this vital, lifesaving work is not recognized as a profession by the Census Bureau. Part of the mission of Clinical Trial Day is to promote this path as a possible career choice. “We are trying to change that as early as high school and college by attending career fairs to make people aware of clinical research (as a career). For me personally, this was something that I fell into when I was at Lenox Hill Hospital many years ago. It’s a career that has been very satisfying and rewarding to me. Many people will tell you it was something they learned about by chance, but they decided to stay in the career by choice,” said Brennan.
On the other side of clinical trials are the patients who benefit. A panel of five participants spoke at Clinical Trials Day about their experiences and answered questions.
Tandica Jackson was diagnosed with acute myeloid leukemia in 2021, when she was 29 years old. She remembers being shocked and confused. “I can recall the doctors coming in one morning to explain all my options, which included a clinical trial for the type of leukemia I had. Even though I was willing to do anything in order to fight this diagnosis, I was very nervous about participating in a clinical trial. The Research Nurse Janice Harmon was great, she had noticed that I was nervous about doing it, so she came back and explained the pros and cons about the Gilteritinib, which was the drug being offered during the trial. After that warm and welcoming conversation with her, and some guidance from my family, I decided to go forward with the clinical trial. I am happy and proud of myself for taking this leap of faith and participating in this trial. It is because of that decision I am here today, in remission, happy and living a grateful life,” said Jackson.
A firm believer in listening to his body, when Alfred Coakley didn’t feel right, he called 911. They recommended that he go to the hospital, where he was diagnosed with Heart Failure and assigned a cardiologist named Dr. Poumpouridis. After his discharge, Coakley continued to see Dr Poumpourdis at her clinic, where she asked if he wanted to be a part of a trial. “She explained that they would provide medication and I might get either the placebo or the active drug. She also informed me that my participation in the study would only be for a specified time. I thought everyone working on the trial was very friendly. One of the key things I can say about everyone I met during this experience is that all of them expressed great empathy,” said Coakley. He believes research is how mankind gains knowledge on overcoming diseases.
James Hall was asked to participate in the Azalea study, which compared the results of anti-coagulation therapies. Since he had had an event of atrial fibrillation and other qualifications, he was eligible to be in the study. “As long as I didn’t have a reaction to the injection components or the antibody, I felt the antibody was being accepted by my immune system. During the study I had laboratory test results that showed the antibody medication seemed to be working. I had a real-life test of the medication when I had an event of atrial fibrillation that lasted for nine days until my cardiac conversion by Dr Donahoe. Since clots in the heart can be caused by Afib, Dr Donahoe performed a Trans-esophageal echocardiogram prior to the conversion. There were no clots found and I was converted back to sinus rhythm without incidence.
I actually look forward to meeting with the study nurses for my monthly injection. The downside is I know I will have to wait for phase 3 to be completed and FDA approval before the medication is available to the public. I will go back to using an Xa inhibitor in the interim,” said Hall.
For more information about the clinical trials available at Feinstein Institutes for Medical Research, visit https://www.northwell.edu/clinical-trials-feinstein call the Office of Clinical Research at (516) 881-7067 or email clinicaltrials@northwell.edu.