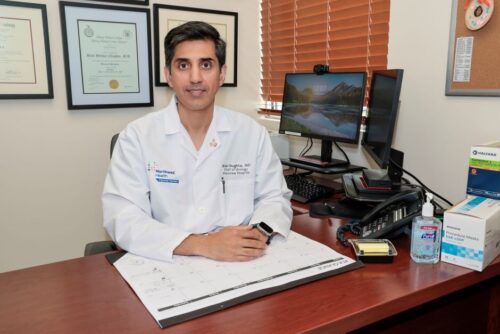
A Northwell Health physician is helping Plainview Hospital make incredible strides for men’s health. Dr. Bilal Chughtai, chair of urology at Plainview Hospital performed the first FDA-cleared iTInd procedure for enlarged prostate; a condition approximately 500 million men worldwide suffer from. This procedure is the first of its kind to be offered on Long Island.
Dr. Chughtai completed his medical degree at State University of New York at Stony Brook, his urologic surgery residency at Albany Medicine Center and his fellowship in female urology, neuro-urology and voiding dysfunction at Memorial Sloan-Kettering Cancer Center and New York Presbyterian Hospital/Weill Cornell Medical College. Operating out of his main office in Syosset, Dr. Chughtai has worked for numerous Long Island medical centers. Continuing his efforts to improve the urolgic health of his community, Dr. Chughtai has led the multi-center trial to bring iTInd to approval in the US.

iTInd, invented by an Israeli company, shows promising signs of eliminating many drawbacks to traditional prostate treatments. iTInd is a small stent placed inside the prostate. Over five days, that small stent reshapes the prostate, making small cuts in it and reshaping it so that the flow of urine is improved, getting rid of the symptoms of urgency frequency, and freeing patients from a lifetime of enlarged prostate medications.
An enlarged prostate can cause a plethora of bothersome urinary symptoms, Dr. Chughtai explained, from urgency and running to the bathroom, going to the bathroom very frequently, getting up at night — often multiple times — to urinate, and in some patients being unable to urinate at all. These issues have effective treatments but notoriously come with side effects that worry potential patients. The iTInd works to eliminate these symptoms while remaining minimally invasive. “The beauty of this new treatment is there’s no associated aromatase function, no change in sexual function, your chance of incontinence or leakage is close to 0 percent,” he said.
The procedure is the culmination of improvements made over decades of research. “We’ve increased the safety of these procedures tremendously, and took it from like an inpatient multi-day admission to a five-minute in-office procedure. And then you come in five days later to have the device removed and that’s it.” Reported benefits of the procedure also include a fast healing time, and no permanent foreign body left behind. “I’ve had very good clinical experience with this procedure where patients are very happy with it,” said Dr. Chughtai.
One such patient is John Franklin, 72, a retired Hospice and Palliative Medicine/Geriatric Medicine physician. Franklin was on the maximum medications for BPH (benign prostatic hyperplasia) and was familiar with several unpleasant side effects. Franklin did not want to undergo a urethral transection or have a foreign device left in his body, since he already had hardware in his heart. When he heard about the iTInd procedure, it seemed like a promising fit.
Franklin flew up from his home in North Carolina earlier this year to have the procedure done. “As a physician myself, I can judge bedside manner immediately, Dr. Chughtai took his time and answered all of my questions,” he said. Franklin was the very first patient to have this procedure done at Plainview Hospital, which was also the first of its kind performed on Long Island. In total, the procedure took about 10 minutes.
Franklin has been very pleased with the results following the procedure, and hopes in the future it will be available in more states. “The nearest place I could get this done was in Atlanta, Georgia… It’s an investment for any hospital to get the equipment. I think that over time it will become more available, it is really minimally invasive.”
This is undoubtedly a sensitive and uncomfortable topic. Dr. Chughtai is familiar with the discomfort and resistance many men face when discussing their health. “I think, unfortunately, there is some stigma around talking about urination where sometimes it falls under the categories of either being humorous or embarrassing. I think I think we have to work to move away from those stigmas and realize these are incredibly common problems. 50 percent of men about the age of 50 — and almost 100 percent of men as they approach their 80s and 90s — have this issue. It’s important to talk to a care professional to at least start that conversation to figure out if you would benefit from some type of evaluation or treatment.”