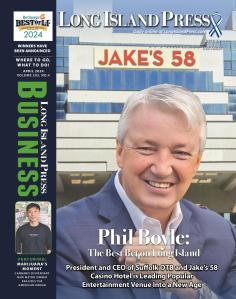
About the Author
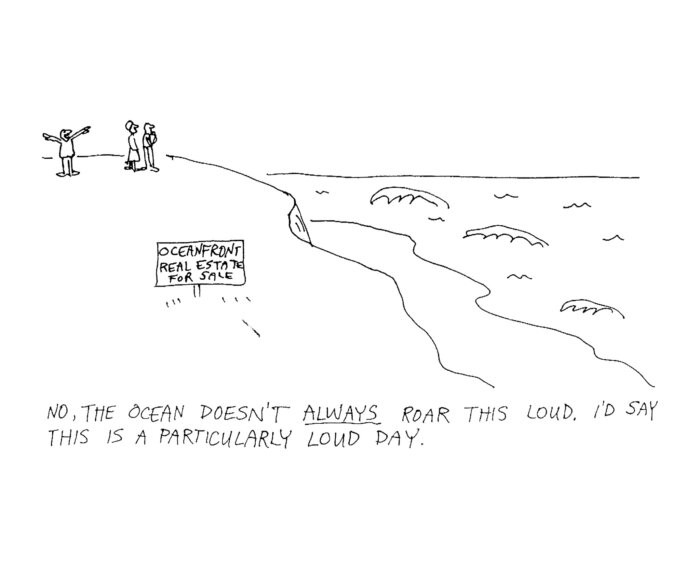
Things to do on Long Island
Today, 1 pm
Today, 1 pm
Today, 6 pm
Tomorrow, all day
Latest News
 Search of Manorville In Connection To Gilgo Beach Murders Expands To North Sea and Halsey Manor Road
Search of Manorville In Connection To Gilgo Beach Murders Expands To North Sea and Halsey Manor Road Selling Weight-Loss And Muscle-Building Supplements To Minors In NY Is Now Illegal
Selling Weight-Loss And Muscle-Building Supplements To Minors In NY Is Now Illegal The Weekender: Things to Do on Long Island This Weekend
The Weekender: Things to Do on Long Island This Weekend These Apps Allow Workers To Get Paid Between Paychecks. Experts Say There Are Steep Costs
These Apps Allow Workers To Get Paid Between Paychecks. Experts Say There Are Steep Costs Stemming The Tide Of Antisemitism On Long Island Amidst Middle East Tensions
Stemming The Tide Of Antisemitism On Long Island Amidst Middle East Tensions