About the Author
Things to do on Long Island
Today, 2 pm
Today, 4 pm
July 26, 7 pm
Sept. 21, noon
Latest News
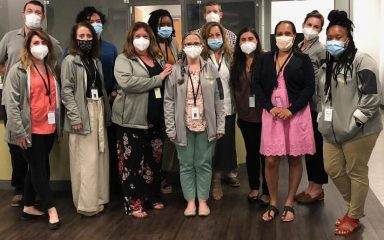
 Northwell wins community health award for serving Long Island’s homeless population
Northwell wins community health award for serving Long Island’s homeless population Top 5 stories in Long Island Press this week: Pro Boxer DWI crash, outdoor concerts and more
Top 5 stories in Long Island Press this week: Pro Boxer DWI crash, outdoor concerts and more Roslyn teen brings smiles with charity SwagAwayAfrica
Roslyn teen brings smiles with charity SwagAwayAfrica Carolyn McCarthy, former Nassau U.S. Rep. and gun safety advocate, dies at 81
Carolyn McCarthy, former Nassau U.S. Rep. and gun safety advocate, dies at 81 Fire rips through 3-story Baldwin apartment building
Fire rips through 3-story Baldwin apartment building