Colorectal (colon) cancer is the second-leading cause of cancer-related deaths in the United States. Colon cancer affects men and women equally. Approximately 50,000 people in the United States are expected to die from colorectal cancer in the upcoming year. The majority of colon cancers evolve from polyps. Colonic polyps, abnormal growths of tissue on the inner lining of the colon, are common findings in men and women 50 years of age and older. Most polyps are not cancerous, but one common type of polyp, known as an adenoma, can develop into colorectal cancer.
Colorectal (colon) cancer is the second-leading cause of cancer-related deaths in the United States. Colon cancer affects men and women equally. Approximately 50,000 people in the United States are expected to die from colorectal cancer in the upcoming year. The majority of colon cancers evolve from polyps. Colonic polyps, abnormal growths of tissue on the inner lining of the colon, are common findings in men and women 50 years of age and older. Most polyps are not cancerous, but one common type of polyp, known as an adenoma, can develop into colorectal cancer.
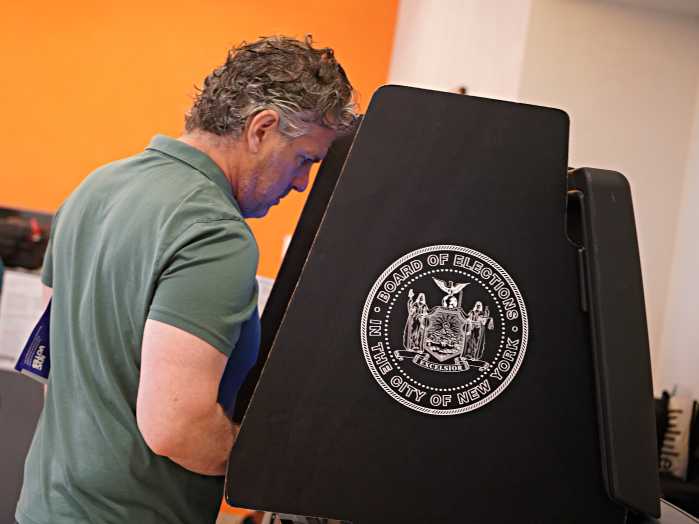
Screening for colon polyps can prevent the development of colon cancer and therefore save lives. In fact, colonoscopy is the only screening test that can prevent cancer from developing. When colon cancer is detected early and treated, the 5-year survival rate is 90 percent. Screening tests for colorectal cancer generally either seek to identify and remove adenomas or examine the stool for signs of early cancer in people who have no symptoms. The current recommendation is that average-risk adults undergo an initial colonoscopy at age 50 to screen for colorectal cancer. A repeat colonoscopy is then to be repeated based upon what was found at 3, 5 or 10 years. If the examiner felt that the preparation was not adequate to properly visualize the colon, a repeat procedure may be recommended sooner.
The preparation for colonoscopy is not always the most pleasant and requires the drinking of a purging agent the day before. There simply is no easy way to clean out the colon so that the examiner can get a good view. Most people think that the preparation is the worst part of the procedure but it really is not that bad, and think of how important a good, clean colon is to visualize polyps. Someone undergoing this procedure certainly wants the best possible visualization to avoid missing abnormalities.
Far and away, colonoscopy has become the accepted standard for colon cancer screening. This test allows for complete visualization of the colon (about four to five feet) and removal of polyps if found. It is well tolerated by patients with an extremely low adverse event rate. Although invasive, sedation is given to ensure that the patient has a good experience. Multiple studies have determined that this test is cost effective and life saving if current guidelines for use are followed. The guidelines for screening are well established and well published. For normal risk individuals, colonoscopy is recommended every ten years beginning at age 50. For African-Americans, the American College of Gastroenterology recommends that screening start at age 45. For those with a family history of colorectal cancer, testing should begin at age 40 or 10 years younger than the age of the youngest affected relative, whichever is earlier. For both average and high risk individuals, all potential pre-cancerous polyps must be removed.
My suggestion to all readers is to consult your physician to discuss colon cancer screening and when it is right for you. With an educated public and a willing medical team, we hope to dramatically decrease the incidence of colon cancer and perhaps even eliminate colon cancer in the future. In New York, we are well on our way to these goals.
David Bernstein, MD, is chief of gastroenterology, hepatology and nutrition at North Shore University Hospital and Long Island Jewish Medical Center.