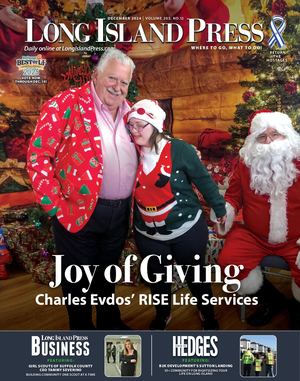
(Credit: NYU Winthrop Hospital)
It has been two months since the deadly novel coronavirus swept New York, killing nearly 20,000 statewide and sickening more than 300,000. At its peak, Long Island hospitals were inundated with sick patients, prompting two of the area’s largest providers, Northwell Health System and NYU Winthrop Hospital, to reconfigure operations to accommodate the spike in hospitalization rates.
NYU Winthrop Hospital, deemed a COVID-19 “Hot Spot” by New York Governor Andrew Cuomo, constructed two outfitted, heated, negative pressure tents on its east campus and repurposed their 3,000-square-foot conference center in the lower level of the hospital to house ICU and ventilated patients. The healthcare system also brought in nurses and doctors from its outside ambulatory centers into the hospital to meet demand.
“When you look at the sheer volume that we faced now that we’re coming down, it gives the impression that we are reopening, but we never closed,” Dr. Marc Adler, chief medical officer at NYU Winthrop, said. “We rearranged to accommodate. Last week was important. We came down to 50 percent off of our peak, but we are still pretty full.”
A Slow Re-Opening
At the height of COVID-19, mothers delivering at Northwell Health’s Huntington Hospital, Southside Hospital in Bay Shore and the Katz Women’s Hospital at North Shore University Hospital (NSUH) in Manhasset and Long Island Jewish (LIJ) Medical Center in New Hyde Park were transferred to postpartum units outside of the hospitals to ensure the safety of the moms and babies, as well as to free up beds for COVID-19 patients.
“By making these changes, we were able to free up hundreds of beds to care for critically-ill patients,” explained Dr. David Battinelli, senior vice president and chief medical officer at Northwell Health. “We are a big operation so there are many, many facets to re-opening. We now have enough space in the hospitals to bring our OB services back up.”
As of April 23, the four Northwell Health obstetric units that were temporarily relocated to make room to care for COVID-19 patients are now back to operating as they were prior to the pandemic. Going forward, women who deliver at each of these hospitals will remain at these facilities for the duration of their postpartum care.
With these milestones being slowly being reached, the next question is what will patient care look like post-peak. It is a road map both hospital systems are rolling out cautiously and deliberately.
“We are past the peak, but we are still very busy,” Battinelli said. “We have more than 500 patients ventilated in our hospitals, we still have more than 2,000 patients with COVID-19 in our hospitals.”
Reallocating Resources
Winthrop is also slowly but surely closing its makeshift surge spaces. As of Friday, May 1, Winthrop is at 56 percent COVID-19, allowing them to return staff brought to their traditional roles in their outpatient facilities. As of publication, the two exterior tents were free of patients (though the structures remain in place should a resurgence occur). The conference center will also continue to remain available to treat COVID-19 patients for the foreseeable future. The goal moving forward, for both the healthcare system is to continue to develop distinctive and separate COVID and non-COVID spaces within the hospitals. The hospitals will also limit cross-contamination, when providers are going from COVID units to non-COVID units.
“We are trying to accommodate new patients that come in, some COVID, and some non-COVID,” Adler said. “We are creating spaces within the hospital that have non-COVID units, as well as COVID units, so we can take care of those patients appropriately.”
Re-Scheduling Surgeries
Battinelli said the next priority is re-scheduling planned surgeries.
“If you have a tumor, for example, and a doctor tells you that you need to have it removed in six weeks, and all of a sudden it becomes week seven or eight, that non-emergency surgery is now becoming urgent,” he said.
Because Northwell performs upwards of 10,000 surgeries annually, the system is backed up by thousands of surgeries, prompting officials to find ways to get surgery centers back up and running.
“That will happen in our ambulatory centers, as well as at Syosset Hospital, because we have been able to move all our patients out of Syosset, empty it, and use surgeries there as soon as possible,” Battinelli said. “We have plans to develop COVID-contained areas.”
Both doctors say there is no doubt social distancing will continue when patients come in for surgeries, or any other doctor’s visit. At Winthrop, there is a separate area within the emergency room for people who are coming in with non-COVID related symptoms. Similarly, if a patient comes in for surgery, the hospital is in the process of creating a non-COVID surgery unit to accommodate them. Right now, Winthrop is not doing elective surgeries, but there are required surgeries that people must undergo, like cancer surgeries.
Procedures and non-elective surgeries have safely been deferred during this time. Urgent surgeries such as cancer surgeries that can’t be delayed safely have been going on throughout the pandemic
“Our ambulatory center is now back available to us,” Adler said. “At one point it was being used to treat COVID patients. Our endoscopy unit was at one point being used for ICU level care so now we can open it up to patients who need endoscopies that cannot be delayed.”
New Protocol Call For In-Person Patient Visits
It is unclear when going to the doctor’s office will be ever like it was pre-pandemic.
“We will certainly be screening patients before they come into the waiting room for fevers, we will screen them for any symptoms,” Adler said. “If they are symptomatic, they will not be seen in the office unless they are severely ill; they will be sent home and have a follow-up telehealth visit. If they are not symptomatic, they will be placed in the waiting room with proper PPE and they will be seen.”
There are many ways to do this, such as not having patients stacked up in waiting rooms and making sure that they install plexiglass barriers—like you see in the pharmacies—between patients and providers. Another way, is to have people wait in their cars instead of waiting rooms.
“It might be impossible for no one in a hospital to have COVID, but we will keep it contained,” Battinelli said. “The data is clear that with the proper amount of PPE, we are safe. Social distancing has worked. PPE has worked. I think you’ll see more safeguards. For example, we have always had Purell dispensers in our facilities. Now, I think you’ll see people using them much more.”

(Credit: Northwell Health)
Telemedicine Is Here To Stay
While both healthcare systems continue to see patients in-person under the proper precautions, telemedicine is here to stay. Doctors and patients have been relying on telehealth and video visits during this time. At Northwell, the system went from having 200 telemedicine providers to thousands during the pandemic. While the NYU enterprise has seen as many as 7,000 telehealth visits a day, about 200,000 telehealth visits total since this started.
“Once people realize they can be seen and treated through telemedicine, you’ll see that it will stick,” Battinelli said. “Telemedicine previously was thought of as a great idea, but no one was willing to pay for it. It is catching on and there will be a large amount of telemedicine in the future.”
No Clear End In Sight
The long-term outlook is subject to testing and preparedness. The hospital systems are working to leave capacity in the form of open beds and a reserve of PPE in the event the virus resurges post-lockdown.
“We don’t know what will happen as things start to open up,” Adler said. “We don’t know if there will be a surge in COVID patients over time. We don’t know if this will be seasonal. We want to be prepared and we don’t want to let our guard down.”
Market research has shown that people are hesitant to leave their houses, they want reassurances and that will happen slowly as testing becomes more widespread.
“We know that people who have antibodies to the virus were exposed, but it is completely unclear what level of immunity they have, though intuitively it would be higher than before they had the antibodies,” Battinelli said. “That doesn’t mean we can open up Madison Square. That is way down the line and probably only when we have vaccines to offer. If a vaccine was developed, that is a year or two years out. There will be vaccines created before then, but test the efficacy of those vaccines is what takes time.”
Morale Is High
On Tuesday, April 21, NYU Winthrop discharged its 750th COVID patient—a remarkable milestone for a hospital that operated with only 511 beds when the first coronavirus patient came through its emergency room doors in early March. And while roughly 2,000 patients with COVID remain in Northwell’s hospitals, the staff is inching even closer to reaching their 1,000th patient released.
“People are happy because we were able to stay safe,” Battinelli said. “We did not have a high infection rate for our staff. We have also seen an incredible amount of support from the media and the community for our frontline workers. That is so encouraging.”