Patients have more choices now than ever before
According to The American Cancer Society, the average risk of a woman developing invasive breast cancer is 13 percent and as a woman ages, the change of having breast cancer increases. Treatment options have advanced over time and the patients—no matter what age— have a variety of options at their disposal.
There are three kinds of treatment pathways for women with breast cancer , which warrants a multi-disciplinary approach. The first being, surgery, the second, radiation oncology and the third, medical oncology. NYU Winthrop Hospital’s Perlmutter Cancer Center has a team of experts—who work together side-by-side to solve the puzzle that is breast cancer.

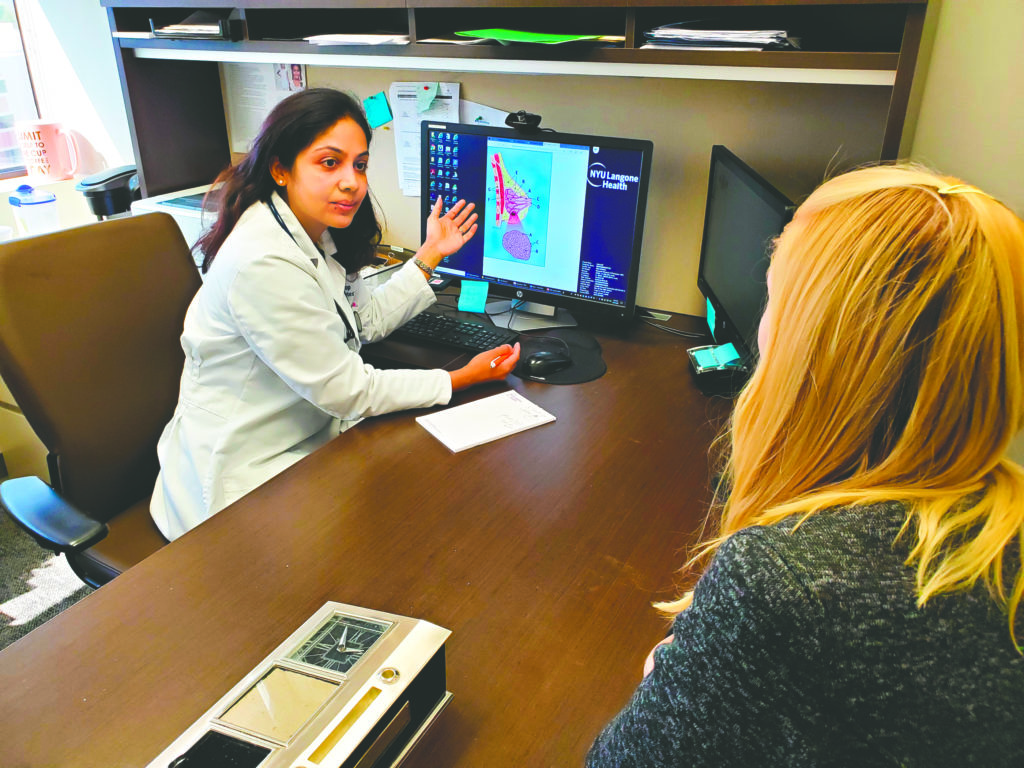
When trying to treat breast cancer surgically, doctors have specific procedures. Dr. Shubhada Dhage is the director of breast surgical services and director of the breast health program at Perlmutter. She said there are two kinds of surgical procedures that can be used as methods to remove the cancer.
“A patient can have what we call breast conservation, which means that we are conserving the breast and the patient can keep their breast and we removed only the tumor,” Dhage said. “The term for that is called lumpectomy. The other type of surgery a patient can have is called a mastectomy—when we remove the entire breast. We can do what’s called an oncoplastic lumpectomy to sort of reshape the breast to make sure that the contour of the breast looks good. We [can] do a lumpectomy or we do what’s called a nipple sparing mastectomy, where we try to hide the scar of a mastectomy and we keep the whole envelope of the breast.”
There have been advancements in the way breast cancer surgery is performed now versus years ago. Dr. Dhage said today’s method is much more effective for the patient.
“One way that has changed how we perform the surgery is before almost every patient had a long wire placed in the breast at the time of surgery in order to help a surgeon do [the] breast conservation or what we call lumpectomy,” she explained. “That patient’s day is somewhat longer. They have to undergo a procedure on the same day of surgery and it’s not as convenient. Now, we can place special markers in the breast, so that in the operating room, we can identify those markers either using a radar device or an ultrasound or a nuclear probe to identify exactly where the tumor is.”
Dr. Amy Solan is a radiation oncologist at NYU Winthrop Hospital and said radiation is performed after surgery—after a lumpectomy or after a mastectomy.

(Photo courtesy of NYU Winthtrop Hospital)
“After a lumpectomy, we will need radiation to that breast to lower the risk of cancer coming back in the breast,” Solan explained. “Although, obviously there are exceptions. After a mastectomy, some patients do not need any radiation. Some patients we see have risk factors in the pathology, like positive lymph nodes or positive margins, large tumor size, things that may indicate a higher risk of cancer coming back either on the chest wall or in the nearby regional lymph nodes.”
Dr. Solan said advancements in radiation treatments are becoming more of a reality for patients.
“Years ago, everybody would get 25 or 30 radiation treatments that are given on a daily basis,” Solan explained. “Now we’re doing our best to do shorter courses. [We do what] we call hypo-fractionation treatments. An example of the hypo-fractionated breast treatment might be 15 to 20 treatments to the whole breast.”
According to Dr. Solan, the Perlmutter Cancer Center at NYU Winthrop Hospital is currently conducting a clinical trial to try and lessen the amount of treatments a patient would receive under radiation.
“We have an open protocol where we’re treating just with a single treatment for selected breast cancer patients,” Solan adds. “This is in conjunction with physicians at UT Southwestern Medical Center.”
Dr. Nina D’Abreo is a medical oncologist and the medical director of the breast health program at Perlmutter. D’Abreo’s role involves not only treating the patients with breast cancer, but she also aides the patients after their treatment.
“As [medical] director most of my function is to actually create processes within the program that allow [survivorship] this to happen,” she explains. “[Our breast health program] allows patients to have a seamless travel journey, right from diagnosis and then survivorship.”
In terms of what a doctor’s role is in medical oncology, Dr. D’Abreo said medical oncologists work to treat the patients entire body.
“We are the providers of what becomes systemic treatment,” she explained. “One way I look at it and I tell my patients, ‘think of it as a seed in the soil.’ The seed is the breast where the cancer is and radiation and surgery kind of work there. We treat the soil. We treat all of you, because cancer cells have a tendency to spread and go other places.”
Dr. D’Abreo added that there are advancements being made in the medical oncology field.
“The clinical trials that are ongoing are really trials to see how we can optimize or make cancer therapy better and minimize the use of chemotherapy, both in the setting of women with what we call early stage breast cancer before it has spread,” D’Abreo said. “But also in women with what we call metastatic or advanced breast cancer. It’s a list of trials, which are comparing either established drugs or drugs that are new in the market. [It’s] experimental in phase two or phase three trials, where we’re trying to make people live longer and to minimize side effects.”