Post-traumatic stress disorder is a mental health condition that can affect anyone who has experienced a traumatic event. For many veterans, especially those who served in combat zones, PTSD can be a lasting and deeply personal challenge. If you’re caring for a veteran with PTSD, you play a vital role in their healing and well-being—and your support can make a profound difference.
Understand What PTSD Is—and Isn’t
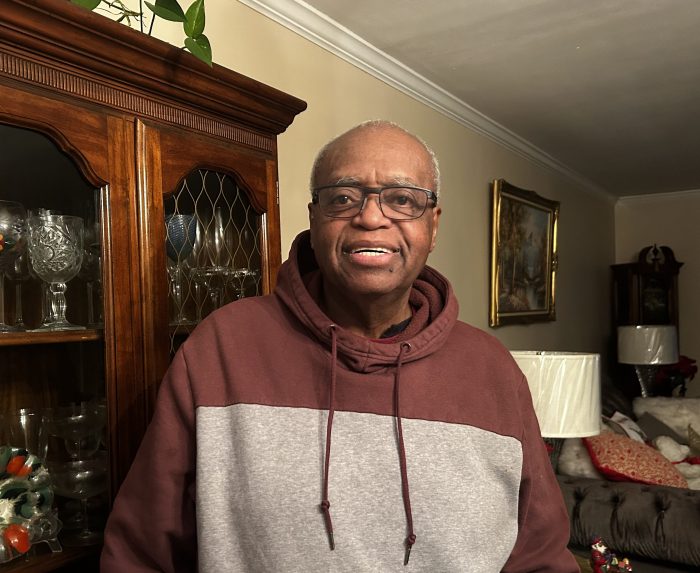
“PTSD is not a sign of weakness,” said Gregg Balbera, president of Right at Home Nassau Suffolk. “It’s a natural response to traumatic experiences, such as combat, injury or witnessing loss.” Symptoms can include:
- Flashbacks or nightmares
- Being easily startled
- Emotional numbness or detachment
- Irritability or angry outbursts
- Trouble sleeping or concentrating
- Avoiding reminders of trauma
When your veteran loved one has PTSD, it affects the entire family. You may notice that they act differently and get angry easily. Your loved one may not want to do things you used to enjoy together. Family members might feel angry about how PTSD is affecting family life or wonder if relationships will ever return to normal. These feelings are natural and expected.
“Understanding that these symptoms are part of a medical condition—not personal behavior or choices—can help you strive for empathy instead of frustration,” Balbera said.
Getting Professional Help
Whether your veteran just returned from a deployment or has been home for 40 years, it’s never too late to get help for PTSD.
PTSD is treatable, but it often requires professional support. Encourage your loved one to speak with a therapist or counselor who specializes in trauma or military mental health. Many veterans qualify for care through the VA, which offers a range of treatments, including mental health assessments, proven medications, psychotherapy (“talk therapy”), family therapy and group therapy. Veterans who can’t easily access VA medical centers can receive counseling over the phone.
Start with VA Mental Health Services at www.mentalhealth.va.gov, or call the Veterans Crisis Line (dial 988, then press 1), or text 838255.
Learn To Listen Without Judgment
“Sometimes the best thing you can do is simply be there,” Balbera said. “Veterans may not always want to talk about what they’ve experienced, but when they do, it’s important to listen without interrupting or trying to ‘fix’ things. Create a safe, nonjudgmental space. Even if they aren’t ready to share, your presence matters.”
Let them know you’re there for them and you’re not going to push them to talk, but that they don’t have to go through this alone.
Create a Calming Environment
Veterans with PTSD may be sensitive to loud noises, sudden changes or crowded spaces. Consider:
- Keeping the home quiet and predictable
- Avoiding loud movies or startling sounds
- Giving them space when they seem overwhelmed
- Respecting their need for routines or downtime
Even small adjustments can help reduce stress and anxiety.
Improving Communication
Better communication can strengthen your relationship with your veteran. The VA offers tips such as:
- Be clear and to the point.
- Be positive. Blame and negative talk won’t help the situation.
- Put your feelings into words. Your loved one may not know you are sad or frustrated unless you are clear about your feelings.
- Don’t give advice unless you are asked.
If communication remains difficult, family therapy is recommended.
Taking Care of Yourself
Helping someone with PTSD can be hard on you. The VA advises that if you are not careful, you may get sick yourself, become depressed, become burnt out or stop helping your loved one.
Here are some ways to take care of yourself:
- Set healthy boundaries.
- Connect with a support group (such as NAMI Family Support Group at www.NAMI.org, VA caregiver resources or local veteran family programs).
- Get enough sleep, exercise and downtime.
- Don’t be afraid to ask for help.
“Caring for someone with PTSD is a journey—and you deserve support, too,” Balbera said.
Know the Warning Signs of a Crisis
If your loved one talks about feeling hopeless, harming themselves, or withdrawing completely from life, it’s essential to take action. Don’t wait. Call the Veterans Crisis Line at 988 (press 1) or call 911 and mention that the person is a veteran experiencing a mental health crisis.
Getting Started With VA Services
If you haven’t already, visit www.ptsd.va.gov for resources, self-assessment tools and links to local VA services.
Recovery is possible, but it takes time. The National Center for PTSD reminds us that “it’s normal to feel helpless at times” and that “things change slowly.” Your patience, understanding and support make a real difference in your veteran’s healing journey.